Recently, I shared this infographic developed by the World Health Organization.
Now, I would love to dig into the study from which this statistic was pulled.
You can read the study in full, here: “On Contribution of Vaccination to Improved Survival and Health: Modelling 50 Years of the Expanded Programme on Immunization.”
I’m going to work backward by sharing the study’s key findings and then digging into the methods. To kick things off, the study centers around the Expanded Programme on Immunization (EPI). The EPI was established by the World Health Assembly in May 1974, marking a proactive commitment to extend the protective benefits of vaccination to all.
Researchers estimated the number of deaths prevented, years of full health gained (i.e., disability-adjusted life-years averted), and years of life gained by vaccination against 14 pathogens between June 1974 and May 2024 in WHO member states: diphtheria, Haemophilus influenzae type B, hepatitis B, Japanese encephalitis, measles, meningitis A, pertussis, invasive pneumococcal disease, polio, rotavirus, rubella, tetanus, tuberculosis, and yellow fever. (There’s a reason they didn’t cover other vaccines, and I’ll get into that shortly.)
Key Findings:
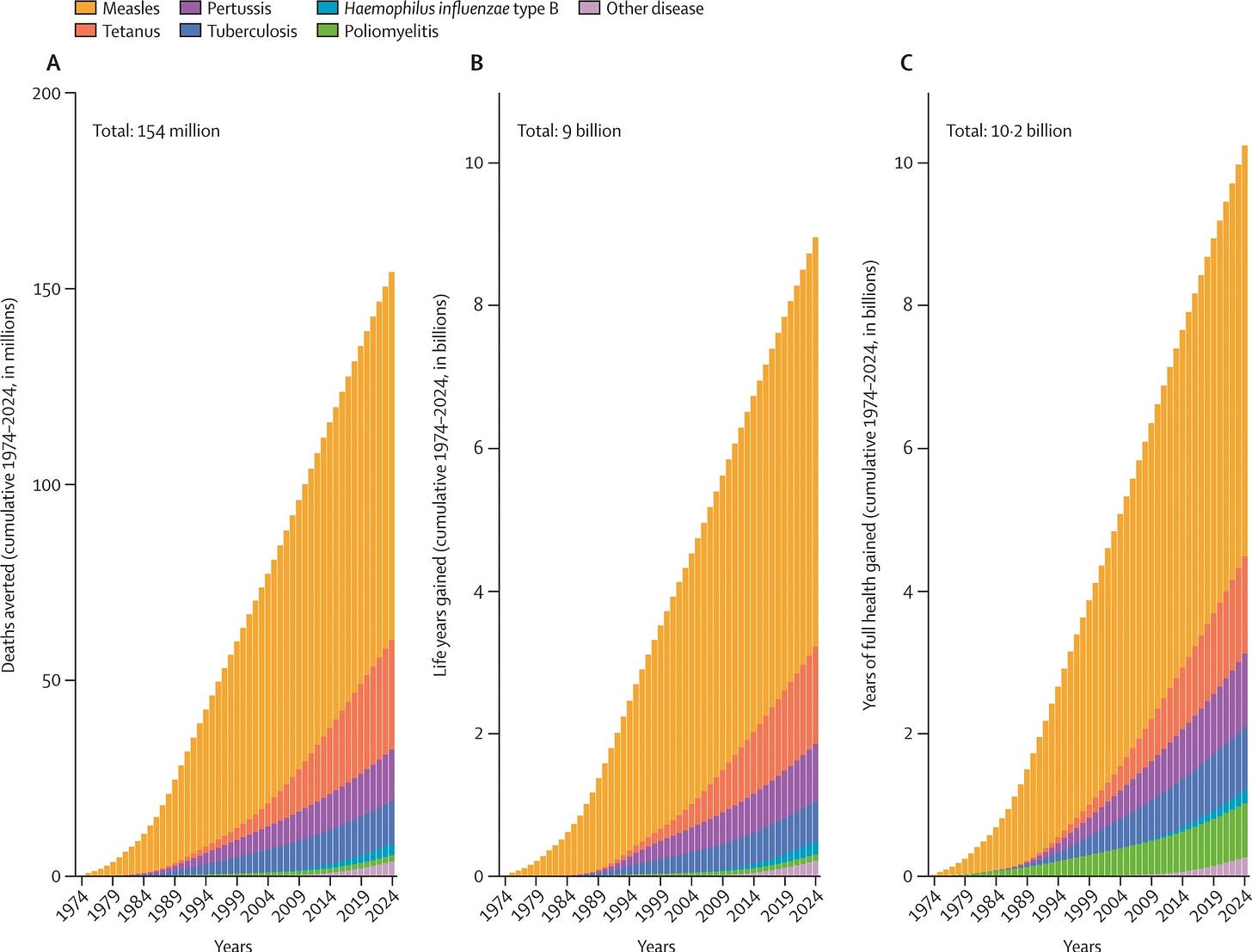
The study estimated that vaccination programs supported by the EPI saved 154 million lives between 1974 and 2024. This includes 146 million children under five, of whom 101 million were infants under one year.
The authors estimated that a child born in 2024 has a 40% increased chance of surviving each year of infancy and childhood compared to if no EPI vaccinations occurred since 1974. These gains are measurable throughout life, even many years after vaccination.
They found that vaccination against measles accounted for the largest number of lives saved (93.7 million), followed by Hepatitis B, diphtheria, and tetanus vaccines.
Beyond just preventing death, EPI vaccinations saved 9 billion life-years and prevented 10.2 billion years of poor health (disability-adjusted life-years, DALYs).
Vaccination has been responsible for about 40% of the significant reduction in infant mortality observed since 1974, with regional variations in the proportion of decline attributable to immunization.
Source: Shattock AJ, Johnson HC, Sim SY, et al. Contribution of vaccination to improved survival and health: modelling 50 years of the Expanded Programme on Immunization. The Lancet, 2024, DOI: 10.1016/S0140 -6736(24)00850-X, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00850-X/fulltext
Let’s get into the methods. The authors used statistical modeling which sounds a little scary and complex and, to be honest, it can be! The study relied on a complex, multi-layered approach, combining different modeling types. The models incorporated data on vaccine coverage, demographics, and disease-specific epidemiology across 194 WHO member states. By examining the relationship between vaccination coverage and vaccine impact in countries where models were available, regional coefficients were developed to predict vaccine impact in countries without direct model estimates. (These are known as imputation techniques and they offer flexibility in addressing gaps in direct data, allowing for broader geographical coverage.)
Let’s discuss the models used:
Dynamic transmission models simulate how diseases spread through populations over time. The study used these for measles and polio, allowing researchers to capture indirect protection (herd immunity) from vaccination.
For diseases where transmission modeling wasn't applicable, static models were used. These models estimate disease burden at a given point in time, incorporating factors like vaccine coverage, death and disability rates, and vaccine efficacy to assess vaccine impact.
Statistical regression helped extrapolate the relationship between vaccine coverage and health outcomes to areas of the world without detailed disease models.
Researchers analyzed how the relationship between vaccination coverage and vaccine impact changed (was it a straight line, or something more complex), allowing more accurate estimations over time and coverage levels.
Interestingly, the study likely underestimates the total impact of vaccination, as secondary effects (like preventing non-communicable diseases) or newer vaccines (like the HPV vaccine) weren't directly considered.
What does this study add? The study's scale is a huge strength. It analyzed 50 years of data, across 194 countries, for 14 pathogens, giving us the most comprehensive analysis of global vaccine impact to date. It combined different model types, allowing for appropriate nuance in evaluating vaccines that prevent disease in individuals and those that also offer community-wide protection through herd immunity. This study provides the strongest evidence to date of the massive contribution of vaccination to global health and supports the central role of EPI in saving lives.
What are the study’s limitations and why didn’t it include vaccines such as those against COVID-19 and HPV?
Complex statistical models like the ones used in this study rely on input parameters and assumptions, creating potential for error propagation that may be challenging to fully trace. This methodology is not perfect. The study also didn't directly capture secondary benefits of childhood vaccinations, like the potential prevention of non-communicable diseases later in life, or factors like improved nutrition in the vaccinated. These benefits could further bolster the findings. Models may have underestimated benefits in cases where a vaccine's efficacy changes based on the age a person is vaccinated or other population-specific factors.
The study authors emphasize that their focus on EPI vaccines means they haven't captured the full impact of immunization. This includes:
Rapidly evolving pandemics like COVID-19.
Vaccines with high year-to-year variation like influenza.
HPV vaccines, which will likely show greater life-saving impact in the future.
Outbreak-specific vaccines (cholera, Ebola).
Vaccines primarily targeting adult diseases.
Vaccines widely used in high-income countries (varicella, zoster, mumps)
Other issues: Since the hypothetical no-vaccination world includes smallpox eradication, the study underestimates the total benefit of vaccination. There might also be a risk of double counting; while they worked to minimize it, some deaths might have been prevented by multiple vaccines, creating a slight overestimate. Also, this study’s focus is on global and regional results. Finely detailed country-specific conclusions are more limited. Finally, measuring impact by year rather than by when someone was vaccinated means they can't fully account for the future impact of vaccines given early in life, especially for diseases occurring later (like hepatitis B). They also had to exclude newer vaccines like HPV due to this limitation.
What about all of the other public health advancements over the past 50 years, surely they contributed? Dozens of people asked this and it is a GREAT question.
Disentangling the contribution of vaccination from other factors like improved nutrition and sanitation is crucial for accurately understanding vaccine impact. Here's how the researchers attempted to control for these confounding variables:
The models themselves accounted for improvements in non-vaccination-related factors that decrease infectious disease cases. For example, the reductions in child mortality over the years influenced the number of measles cases the model would predict, even without vaccination. This way, researchers could isolate the additional decline in cases specifically attributable to the vaccine.
The researchers analyzed how the proportion of infant mortality reduction attributable to vaccination varied across regions. Regions with lower baseline sanitation and nutrition likely showed a smaller relative contribution of vaccination compared to areas with better initial health infrastructure.
The types of models used varied by disease, which implicitly captures some of these factors. For example, measles spreads person-to-person, so improving sanitation would only minimally reduce measles cases, highlighting the vaccine's role when we see significant declines. Conversely, diseases spread through fecal-oral transmission, like tetanus, would show less additional benefit from vaccination in settings where clean water and improved sanitation rapidly reduced transmission on their own.
But the reality is that even with careful modeling, it’s impossible to completely isolate the impact of vaccines for a variety of reasons. For starters, improvements in nutrition, sanitation, and healthcare often go hand-in-hand with vaccination programs. Vaccinations are part of a larger public health system, making it difficult to isolate the exact contribution of each component. Historical data on factors like sanitation might be less granular and reliable than vaccination coverage records, making it harder to incorporate them as precisely into the models.
While some uncertainty remains, the enormous impact demonstrated in the study, even after accounting for external factors, strongly supports the conclusion that vaccination programs played a massive role in improving global health over these past 50 years.