The Importance of Community Water Fluoridation: Evidence and Impact
Using Data Visualization To Tell The Story
Let’s Start With a History Lesson.
Deaths from dental abscesses are so rare today that it's difficult to imagine they were once a major killer. When the London Bills of Mortality began recording causes of death in the early 1600s, "teeth" consistently ranked as the fifth or sixth leading cause of mortality. Even into the early 1900s, dental infections proved fatal in 10-40% of cases. This dramatic transformation in dental mortality was driven largely by our understanding and use of fluoride, a discovery that began with a curious observation in Colorado.
The Colorado Discovery and Early Research
In the early 20th century, dentists in Colorado noticed something puzzling. Many residents had large, permanent brown stains on their teeth - an aesthetically concerning condition later identified as fluorosis. Yet, notably, these same residents showed remarkably low rates of tooth decay. This observation prompted scientists to investigate, and by 1931, they had pinpointed high levels of naturally occurring fluoride in the drinking water as the cause of both the staining and the cavity protection. Huzzah!
Dr. H. Trendley Dean, head of the Dental Hygiene Unit at the National Institute of Health, led groundbreaking research to determine the optimal fluoride level that would prevent cavities while avoiding fluorosis. His careful studies in the late 1930s revealed that fluoride concentrations up to 1 part per million (ppm) in drinking water could achieve this balance.
Landmark Studies Prove Effectiveness
This discovery led to two pivotal studies that would revolutionize public health. The Grand Rapids Fluoridation Study, initiated in 1945, was the first long-term evaluation of water fluoridation's effects. Over 11 years, researchers documented a 60-65% reduction in dental caries among children who consumed fluoridated water from birth. Even children with pre-existing teeth showed benefits, experiencing reduced decay and fewer missing or filled teeth.


The Newburgh-Kingston study in New York provided further validation. Children aged 6-9 years showed 55% fewer decayed, missing, and filled permanent teeth compared to the control city of Kingston. The impact extended across age groups, with 10-12 year olds demonstrating 43% fewer affected permanent teeth. Among the youngest children, 5-year-olds showed 59% fewer decayed deciduous teeth, though this advantage decreased to 12% by age 8.

Implementation and Growth
Following these successful trials, the U.S. Public Health Service endorsed community water fluoridation, leading to widespread adoption. By 1960, approximately 50 million Americans had access to fluoridated drinking water. This number grew to encompass half of all Americans by 1980, and by 2010, two-thirds of Americans (over 200 million people) had fluoridated water. However, recent years have seen some retreats - by 2022, coverage had decreased to 63% as various local governments discontinued fluoridation programs (more on this in a sec).
Modern Evidence
The evidence for fluoridation's effectiveness has only grown stronger with time. Modern studies continue to validate its impact - when Calgary stopped fluoridating its water in 2011, researchers documented poorer dental health in children compared to Edmonton, which maintained fluoridation. Similarly, after Juneau, Alaska removed fluoride in 2007, cavity rates increased. These natural experiments add to the extensive body of research supporting fluoridation's benefits.
Current Landscape: Regional Patterns and Trends
Water fluoridation coverage across North America remains uneven. While some Canadian regions like Ontario and Manitoba maintain high rates, others like Quebec and British Columbia have very low coverage. These disparities directly affect dental health outcomes across regions.

In the United States, implementation varies significantly by state and locality. From 2016 to 2020, some states strengthened their fluoridation programs while others retreated:
Pennsylvania showed encouraging growth (+5.4%), reaching 60% coverage
Delaware's significant decline (-11.4%) reduced coverage from 87% to 76%
Louisiana, already among the lowest-ranked states, decreased further from 44% to 38%
The Impact on Dental Health and Care
Analyzing the relationship between fluoridation levels and dental visits reveals an interesting pattern. The most significant improvements occur in the transition from low to medium fluoridation coverage:

By Fluoridation Level:
Low (0-25%): 14.01% average fluoridation, 72.05% dental visits
Medium (51-75%): 64.04% average fluoridation, 66.02% dental visits
High (76-100%): 88.81% average fluoridation, 65.81% dental visits
Access and Equity: Understanding State-Level Disparities

Paradoxically, some states with low fluoridation rates show higher dental visit frequencies. Hawaii, with less than 10% fluoridation coverage, reports nearly 10% more dental visits than the national average. Conversely, highly fluoridated states like West Virginia and Kentucky show 7% fewer dental visits than the national average. This suggests that while fluoridation is crucial for dental health, other factors significantly influence access to dental care.
The Economic Case for Fluoridation and Income-Based Disparities
Community water fluoridation (CWF) represents one of public health's most cost-effective interventions. Like adding iodine to salt or folic acid to grains, it ensures universal access to an essential health measure. While suggesting people simply "buy fluoride toothpaste" might seem reasonable, this overlooks the reality that dental care remains inaccessible for many.

The income bracket analysis reveals striking disparities between households earning <$15k versus >$50k annually:
Lower-income areas show reduced access to regular dental care
Limited ability to purchase fluoride products consistently
Barriers to proper oral hygiene education and resources
These disparities highlight why community water fluoridation's cost-effectiveness is particularly important from a public health perspective. While the upfront costs of implementing and maintaining fluoridation systems can seem significant to local governments, the long-term economic benefits are substantial and disproportionately help those who face the greatest barriers to dental care.
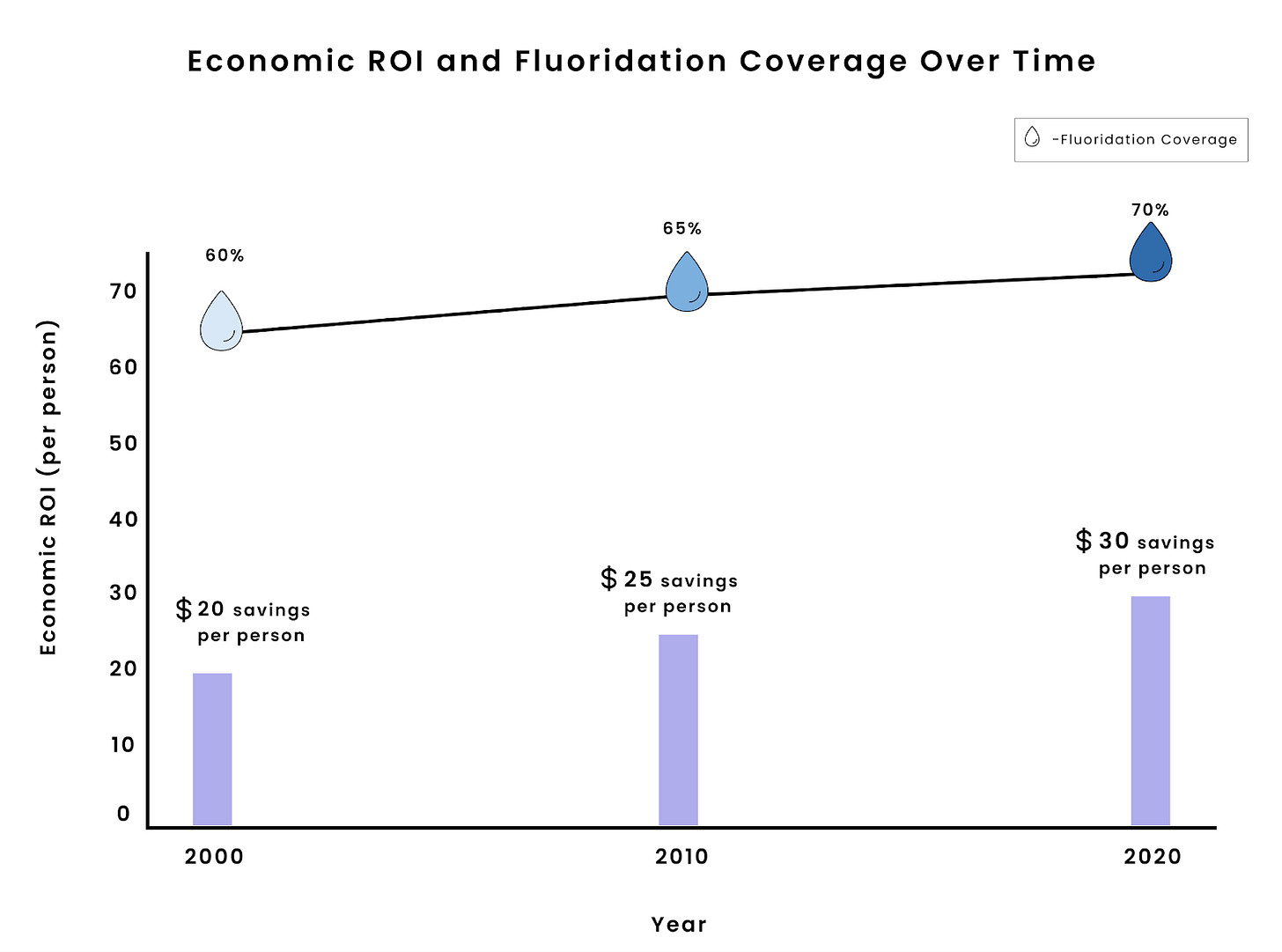
The return on investment has grown consistently:
2000: $20 savings per person (65% coverage)
2010: $25 savings per person, nearly $6.5 billion nationally
2020: $30 savings per person (70% coverage)
Educational Achievement and Dental Care
Education levels strongly influence dental care access, regardless of fluoridation status. Let's examine the patterns in both high and low fluoridation areas:

In states with high fluoridation rates:
College graduates: 90% dental visit utilization
Less than high school education: 44% utilization
The gap represents more than half of recommended dental visits

Image created by Unbiased Science. Data source: Oral Health Data: Explore by Topic | DOH | CDC.
In states with low fluoridation rates, the educational divide persists:
College graduates maintain high utilization at 90%
High school diploma holders miss 50% of recommended visits
Those with less than high school education show slightly better access than in high-fluoridation states, missing only 38% of recommended visits
These patterns demonstrate that while fluoridation is important, educational disparities in dental care access persist regardless of fluoridation status.
Racial Disparities in Access
National data reveals persistent racial disparities in dental care access relative to the national average:
White: +3.6 percentage points
Black: -4.5 percentage points
Hispanic: -7.4 percentage points
Multiracial: -6.1 percentage points
Other: -2.7 percentage points

State-level analysis shows varying degrees of disparity:

North Dakota: highest inconsistency (SD 6.82)
Pennsylvania: largest gap (36.9 points)
Massachusetts and Oregon: more equitable access patterns
Prevention Methods: A Comparative Analysis

Community water fluoridation stands out for its unique advantages:
Universal reach without requiring individual action
Consistent delivery regardless of dental care access
Strong evidence base
Cost-effective community-level implementation
While CWF significantly improves dental health outcomes, it cannot completely close gaps created by broader systemic inequities. This research underscores the need for comprehensive approaches combining fluoridation with other interventions to address persistent disparities in access and outcomes.
Final Thoughts
The story of fluoridation represents both a remarkable public health achievement and an ongoing challenge. From the early observations of brown-stained teeth in Colorado to today's sophisticated understanding of dental health inequities, we've learned that simple, universal interventions can dramatically improve population health. Yet our data reveals that fluoridation alone cannot overcome the deep-rooted disparities in dental care access. As some communities retreat from water fluoridation despite strong evidence of its benefits, we risk widening these gaps further. The path forward requires maintaining this cornerstone of dental public health while simultaneously addressing the broader systemic barriers that keep many Americans from accessing adequate dental care.
After all, the promise of fluoridation was never just about preventing cavities - it was about ensuring that everyone, regardless of income, education, or race, could maintain basic dental health. That promise remains as relevant today as it was when researchers first discovered fluoride's remarkable properties in the waters of Colorado Springs.
Also, isn’t data visualization neat?
Stay curious,
Unbiased Science
P.S. We have covered fluoride extensively in past newsletters. Check them out here:
1. Deep dive on the NTP report that claimed to find an association between high levels of fluoride and decreased IQ.
2. Discussion of the federal ruling that the EPA must further investigate the impacts of fluoride.
3. The implications of community water fluoridation on health equity.





Dental visit probably don't correlate well with poor dentition. Much higher visits in NJ and HI vs WV are likely due to high number of dentists/access.
https://expressdentist.com/dental-health-ranked-by-state/