Note: This is a paid partnership with Champions of Vaccine Education, Equity, and Progress (CVEEP).
New Report on the Challenges of Shared Clinical Decision-Making for Vaccines
This week Champions for Vaccine Education, Equity, and Progress (CVEEP) published a white paper that takes a close look at a concept in the vaccine space, known as shared clinical decision-making (SCDM). SCDM recommendations for vaccines differ from other recommendation types and, while not inherently problematic – according to CVEEP’s recent findings—can create challenges for providers and patients, and ultimately impact uptake.
First things first! What is SCDM?
Shared clinical decision-making is a collaborative process where healthcare providers and patients work together to make medical decisions, considering scientific evidence, clinical expertise, and patient preferences.
This approach is particularly relevant for certain immunizations where individual factors may influence the decision to get vaccinated. In these cases, providers discuss the benefits, risks, and patient-specific factors to help individuals make informed choices about vaccination. This process aims to balance population-level recommendations with individual circumstances and values.
So, what are SCDM recommendations, exactly? And why is it important to understand the implications of these types of recommendations?
BACKGROUND ON SHARED CLINICAL DECISION-MAKING
In the United States, the Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) approve and recommend vaccines to prevent and control infectious diseases. Following FDA approval, the CDC’s Advisory Committee on Immunization Practices (ACIP) develops recommendations based on factors like disease epidemiology, vaccine safety and efficacy, population-specific considerations, public health impact, and health equity. The CDC then establishes immunization schedules based on ACIP’s recommendations.
ACIP uses three primary recommendation types:
Routine (age- or risk-based): A recommendation that a vaccine be administered to everyone in a particular age group of risk category.
Catch-Up: A recommendation that a vaccine be administered to individuals who missed a vaccine when they were younger, ensuring they are up to date with the current immunization schedule. This type of recommendation can also be made when a new vaccine is approved by the FDA, to ensure that individuals who either were not previously vaccinated against a particular disease or who received an earlier version of the vaccine, can receive the new vaccine to benefit from its improved protection
Shared Clinical Decision-Making (SCDM): A recommendation that the decision to vaccinate be made jointly by the healthcare provider and the patient with consideration for the individual benefits and risks.
As outlined above, SCDM is a relatively new language, introduced in June 2019 as an evolution of the “Category B” recommendation. Unlike routine recommendations, SCDM vaccines are administered based on patient-provider discussions and individual preferences. ACIP issues SCDM recommendations when there is an individual-level benefit but uncertainty about broad benefit.
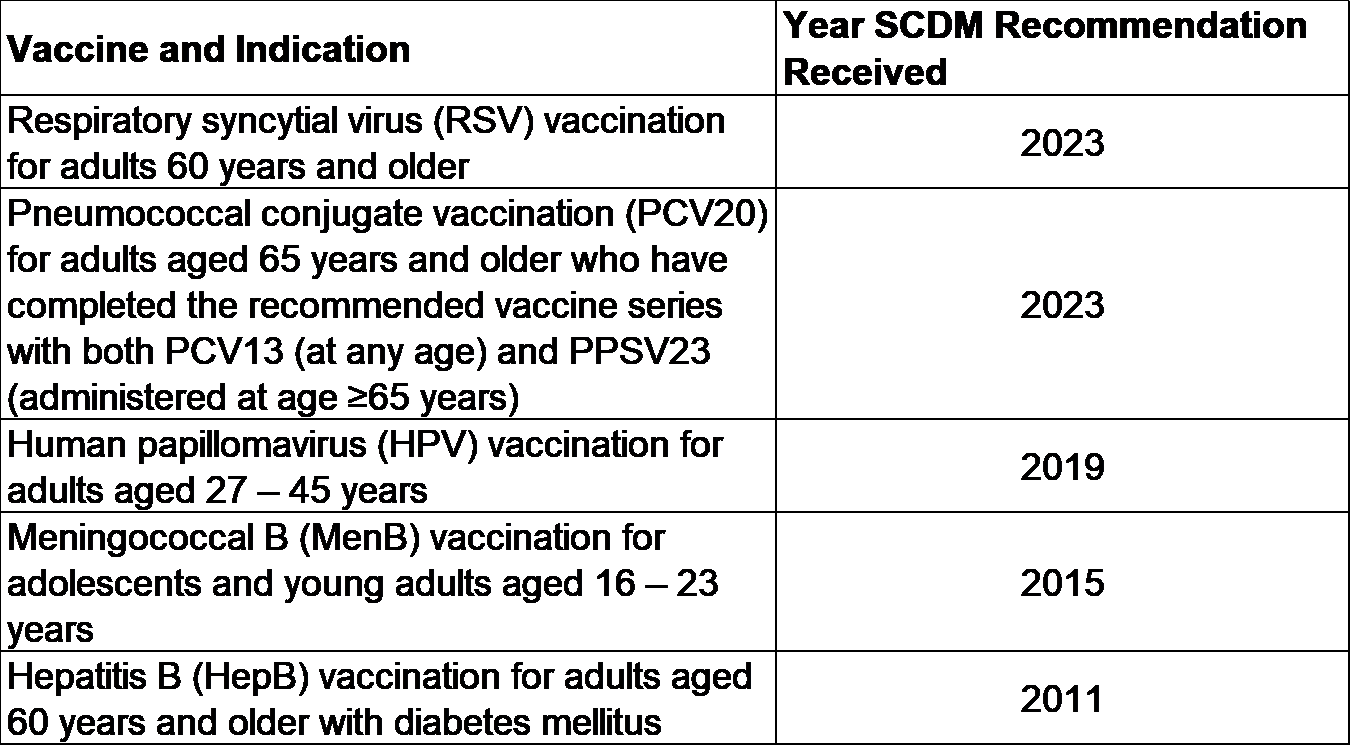
Currently, five vaccines have SCDM recommendations—and notably, 75% of these vaccines impact older adult populations:
SCDM can create complexities and hurdles that impact providers, patients, administration, reimbursement, and vaccine uptake. Moreover, these challenges may be particularly detrimental to underserved groups, exacerbating health disparities and undermining efforts to ensure broad vaccine access.
The below section summarizes the key challenges related to SCDM vaccine recommendations that were outlined in the CVEEP white paper that was published earlier this week.
SCDM recommendations can further complicate patient-provider communications, requiring increased time and resources from providers as they balance the need to provide a comprehensive recommendation while addressing diverse beliefs, varying health literacy, and increasingly widespread mistrust and misinformation. Healthcare providers (HCP)—including those in physician offices and at the pharmacy—play a critical role in providing vaccination services to their communities, and data show that communication between HCPs and patients is one of the most important factors shaping individuals’ trust and openness to vaccination. However, initiating and navigating conversations around vaccines, especially those not routinely recommended, can be challenging and time-consuming and SCDM can present several issues for providers. This has become especially true in the context of the COVID-19 pandemic, as decisions about vaccinations have become increasingly personal and politicized.
A SCDM recommendation can make patient-provider communications about vaccines even more complex, requiring increased time and resources from providers as they balance the need to provide comprehensive patient education with limited consultation time, resource constraints, diverse cultural beliefs, varying health literacy levels, and increasingly widespread dissemination of misinformation and mistrust in vaccines. All of these factors complicate the decision-making process and can stand in the way of providers’ ability to offer strong, personalized, and effective vaccine recommendations.
SCDM emphasizes patient responsibility, placing increased importance on health literacy, culturally competent resources, and consistent healthcare touchpoints. This increased responsibility can impact vaccine uptake, especially among vulnerable and underserved populations. Because of the lack of standard guidelines, providers may inconsistently facilitate SCDM discussions, leading to disparities in vaccine awareness and uptake. A significant number of Americans face barriers to primary care, with many lacking a regular healthcare provider—an issue that disproportionately affects underserved populations. Reliable access to primary care, continuity in patient-provider relationships, and the availability of culturally competent care are vital for vaccine uptake, particularly for SCDM vaccines that require more nuanced counseling. When these factors are not established, individuals who are eligible and could benefit from vaccination are likely not receiving vaccination services.
SCDM adds complexity to vaccine management, impacting forecasting, administration, and creating financial and logistical barriers that could in turn hinder vaccine uptake. These challenges can present financial and logistics barriers that can disincentivize the stocking of SCDM vaccines, which in turn can lead to referrals to secondary sites, and even reduced recommendations, both of which ultimately have the potential to erode uptake rates. Further, SCDM recommendations are often not supported by current electronic health record (EHR) systems making it more difficult for vaccine administrators to assess vaccination opportunities and to take and understand drivers of vaccine uptake.
Current reimbursement models do not fully account for the complexities or additional resource requirements associated with SCDM vaccines, and as a result integration of SCDM may be financially challenging for many vaccine administrators. As a result, vaccine administrators are often faced with significant challenges related to reimbursement and infrastructure when administering vaccines with this recommendation. A lack of adequate and appropriate incentives for SCDM means that integration of SCDM into provider practices and other vaccination settings may be financially challenging. These issues stand to impact patients from all demographic groups but -- as is often the case -- gaps in reimbursement can be especially pronounced in settings that serve lower-income and underserved populations and, therefore, these challenges may be particularly burdensome for already vulnerable populations.
The challenges associated with SCDM impact many patient populations but may be especially detrimental to underserved groups, which in turn stands to exacerbate existing health disparities and undermine efforts to ensure broad vaccine access. Underserved populations often face disproportionate barriers related to social determinants of health such as limited health literacy, inconsistent healthcare access, and logistical challenges in receiving vaccines. Without standardized guidelines and adequate support systems, the implementation of SCDM can lead to inconsistent recommendations and missed vaccination opportunities, further entrenching health inequities and compromising efforts to achieve equitable vaccine distribution and uptake.
CONCLUSION AND TAKEAWAYS
Vaccines are a critical public health intervention, but their benefits can only be realized with broad and equitable access and administration. At a high level, CVEEP’s white paper highlights that the complexities of SCDM recommendations can add challenges for providers, patients, vaccine management, and reimbursement. These hurdles can be particularly burdensome to underserved populations and, in turn, may exacerbate health disparities. Addressing these challenges is essential to ensuring equitable vaccine access and improving overall health equity.
To learn more and access the full report visit: https://cveep.org/wp-content/uploads/2024/06/CVEEP_SCDM.pdf