In December 2021, Paxlovid received Emergency Use Authorization by the FDA as treatment for COVID-19 illness. Intended for adults and children over 12 years old who have tested positive and who are at increased risk of severe disease, Paxlovid has shown promise as a means of reducing risk of hospitalization and death from COVID-19.
Paxlovid is a prescription antiviral treatment composed of two drugs; the nirmatrelvir works to suppress replication of the SARS-CoV-2 virus and the ritonavir slows the body’s metabolism of nirmatrelvir. In tandem, they work to treat COVID-19 infections and result in a reduced risk of hospitalization and death over a five-day course of treatment. Treatment with Paxlovid must begin within five days of symptom onset and is not recommended for those taking certain medications due to drug interactions.
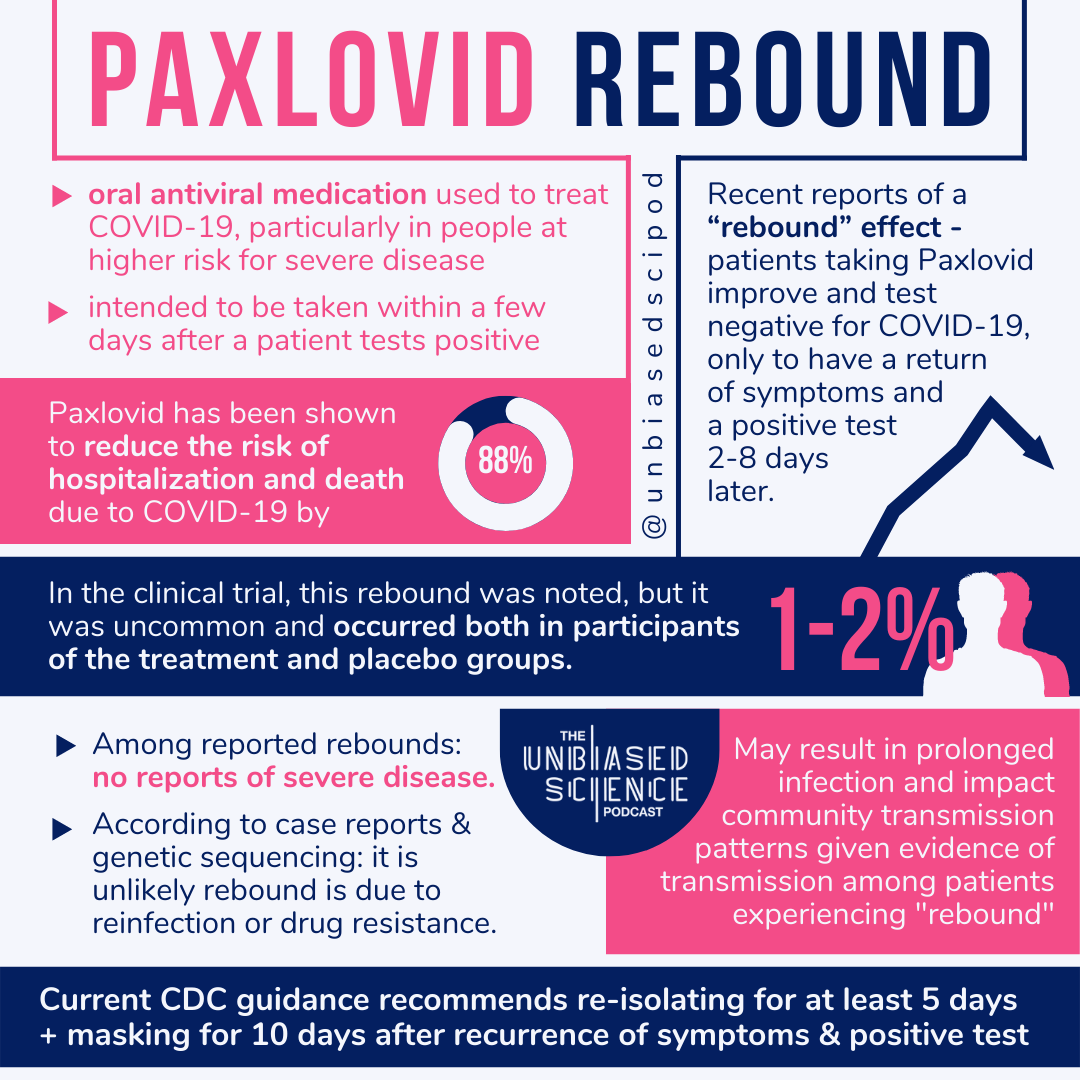
Recently, Paxlovid has made headlines as reports have come in about individuals having a “rebound” post treatment. In these instances, individuals have reported a recovery period including improvement in or resolution of symptoms and even negative tests, followed by a return of symptoms and positive tests two to eight days later. This effect occurred regardless of vaccination status. Among those who have reported a rebound post Paxlovid treatment, there have not been any reports of severe disease or deaths.
While this “rebound” phenomenon was noted in the initial clinical trial, it only occurred in one to two percent of patients. Interestingly, the patients who experienced a rebound included both those who received Paxlovid treatment and those who served as placebo-treated controls. Investigations are ongoing to determine how often these events are occurring outside of the trial context. Pfizer has a current trial investigating how those without increased risk of severe disease react to treatment, with study completion planned for this upcoming fall.
The CDC and FDA do not currently recommend re-administering Paxlovid in the event of a rebound. Instead, healthcare providers are advised to report these cases and continue to monitor patients’ symptoms. Due to evidence of COVID-19 transmission from patients experiencing this rebound, current CDC guidance recommends re-isolating for at least five days (can discontinue isolation after five days if no symptoms) and continuing to mask for 10 days post recurrence of symptoms and positive test. It is not yet known whether the Paxlovid treatment-associated rebound represents a greater or lesser chance of transmission as compared to the pre-treatment infection status.
Although Paxlovid is a tool intended to help those most vulnerable to severe disease, there are anecdotal reports that it may be difficult to find and obtain. As of today, July 18, 2022, the United States Department of Health and Human Services reports that about 1.2 million Paxlovid treatments are available in the U.S. “Test to treat” centers have opened through many local pharmacies and community centers in order to provide increased access to treatments such as Paxlovid. A treatment locator tool is available to find such availability near you.
Another available FDA-authorized treatment is Veklury (remdesivir), although it is not often preferred to Paxlovid on the basis of practicality. Veklury must be administered through an IV infusion for three consecutive days, which can increase the treatment burden for many patients. On the other hand, Paxlovid is an oral medication that is taken for five consecutive days, making the treatment plan much more manageable and accessible for many populations. For this reason, the FDA “does not consider Veklury to be an adequate alternative to Paxlovid for this authorized use.”
The cause of the reported post-treatment rebound effect is a difficult puzzle to solve; at this point in time, the reason for the Paxlovid rebound is unknown. According to the CDC, the reports of Paxlovid rebound do not suggest reinfection with the virus post treatment or development of resistance to treatment, although investigations are ongoing.
Some proposed theories include:
This rebound effect is part of natural history of disease and is more likely to be noticed when an individual is taking a medication that they expect to make them better.
That Paxlovid works too quickly, not giving the individual’s immune system a chance to properly respond. When treatment is complete, some remaining virus may have survived and trigger reinfection.
Notably, the proposals in the list above are simply speculation and theories not yet backed by much, if any, evidence. With more data and time, we hope to learn the mechanism behind such an effect. In the meantime, Paxlovid is still determined by the FDA to be safe and effective in preventing hospitalization and death among those with COVID-19 infection.
Additional contributors: