IUD Insertion Pain
Why it's not "just a little discomfort" for many—and what to ask for
Melissa took 800 mg of ibuprofen to prepare for her IUD placement appointment. She had been told to expect some discomfort and cramping, but nothing prepared her for the sharp and stabbing agony that came next. She left her appointment feeling shocked and traumatized, wishing someone had warned her or offered some relief. “I can confidently say it was the worst pain I’ve ever experienced,” she recalls. In an ideal world, getting an IUD would be a quick, routine procedure with minimal discomfort. In reality, Melissa’s story is far from unique.
IUDs 101!
What Are IUDs?
Intrauterine devices (IUDs) are small, T-shaped contraceptive devices inserted through the opening of the cervix and placed inside the uterus by a healthcare provider. Once positioned in the uterus, they prevent pregnancy either by releasing hormones or by creating a sperm-toxic environment. They are among the most effective long-acting reversible contraceptives (LARCs), with typical-use failure rates well under 1%. IUDs offer years of pregnancy prevention (typically 3–10 years, depending on type) without the daily effort of pills or other per-use methods. There are two main types: hormonal IUDs (containing a progestin, which blocks sperm by thickening the cervical mucus), and the non-hormonal copper IUD (which creates a sperm-toxic environment).
Why Does Placement Sometimes Hurt So Much?
Several physiological and personal factors can influence the ease or pain of an IUD insertion:
Nulliparity (no prior vaginal birth): Women who have never delivered vaginally (this includes women who’ve only had prior cesarean births) report higher pain during insertion than women who have given birth vaginally.
History of dysmenorrhea: Women who experience very painful periods tend to report more pain with IUD placement.
Timing and anatomy: Inserting an IUD long after a pregnancy, or at a time when the cervix is less naturally open (for example, outside of menstruation), can make insertion more uncomfortable.
Type of IUD: Insertions of the levonorgestrel (hormonal) IUD, which has a slightly thicker inserter, are sometimes reported as more painful than copper IUD insertions.
Anxiety and Fear of Pain: A patient’s mental state and expectations have a huge impact on actual pain experienced (more on this later in the Fear-Pain Cycle).
“I Wasn’t Prepared for That Level of Pain”
So if IUDs are so safe and effective, why are there so many horror stories? The answer is in women’s lived experiences: many women find themselves completely overwhelmed by the excruciating pain and sense of betrayal after being told to expect some discomfort. They describe feeling “an explosion of cramps,” sensations of “pulling, pushing and slicing,” or as if they were “cut or ripped open inside,” according to accounts compiled by The Washington Post. Local anesthetics and other medical options are available for IUD placement (more on this later!). Still, many women say they weren’t offered more than ibuprofen to manage their pain, despite evidence that NSAIDs alone aren’t very effective for insertion pain.
These “shock and betrayal” stories highlight a clear disconnect in evidence-to-practice: women’s pain has been underestimated and undertreated by a system that is meant to protect them. In fact, research shows that clinicians consistently underestimate the pain of IUD insertion, where one popular study found that patients’ average maximum pain was nearly double the pain that clinicians estimated (patients rated it about 65 on a 100-point scale, whereas providers guessed ~35). With IUD insertions, the tendency to trivialize the description of pain may be well-intentioned. As some doctors in Wisconsin say, they’re taught to try to provide comfort and strike a balance between preparing patients and not scaring them. Unfortunately, this has often led to women being blindsided and traumatized.
Pain is complicated, shaped by more than just the procedure itself. One woman discovered years later that the searing pain she had felt likely came from internal scarring in her uterus, possibly caused during insertion or removal of a previous IUD. Another shared how her IUD hadn’t been placed properly and was left “dangling” inside her. Others point to systemic issues like racial dynamics: one Black woman recounted that three White providers either inserted her IUD incorrectly or dismissed her concerns, whereas her woman-of-color OB/GYN finally listened and tailored care to her needs. The variability in pain isn’t just physiological; it’s often about whether someone feels heard, seen, and believed.
“It Wasn’t That Bad”: The Other Side of the Story
Still, it’s important to acknowledge that not everyone’s experience is horrific. Many people report that while the procedure was uncomfortable, it was quick and far less painful than feared. For example, one IUD recipient from Charleston compared it to strong period cramps but “nothing unbearable,” emphasizing that the pain, while present, was manageable for her. Another person wrote that they’d heard endless horror stories online, but their actual appointment was “super quick, surprisingly painless.” A Wisconsin OB-GYN noted that most of her patients ultimately compare the feeling to an intense period cramp, with a few even pleasantly surprised that it wasn’t as bad as they anticipated.
“Can’t Be Impacted by Political Changes the Way Pills Can”
Crucially, even those who suffer during insertion often still appreciate their IUD afterward. Melissa, whose story opened this article, said she was left shocked and traumatized, but still glad to have the IUD in the end. In a 2018 study of young women aged 14 to 24, participants reported higher pain than expected during insertion. Yet, over 75% said immediately afterward– and again six months later– that they’d recommend the IUD to a friend. Another woman described three miserable weeks of cramps and sleepless nights following insertion. But now? “Absolute bliss,” she said. “I’d happily take that 3 weeks of hell again for the amazing feeling I have now, and I won’t need to change this IUD for 5 years! It’s the best decision I ever made!”
These stories are a reminder that autonomy matters. One woman said she chose an IUD because she wanted something highly effective “that can’t be impacted by political changes the way the pill can”. Another told Allure that she got her IUD in 2016 after Trump was elected, and with reproductive rights under attack again, she’s glad she did. In fact, IUD insertion rates rose more than 21% during the first month of Trump’s presidency, according to a Brigham and Women’s Hospital study published in 2019. Although the pain is steep, IUDs are still tools for control, especially when other reproductive rights feel increasingly out of reach.
The Pain-Fear Cycle
Ironically, high levels of fear and anticipated pain surrounding IUD placement aren’t just stressful; they may directly increase the pain experienced. A 2018 study of over 1,100 first-time IUD users found that for every one-point increase in expected pain (on a 10-point scale), reported pain rose by nearly 19%. Furthermore, concern about insertion pain is among the most common reasons patients opt for other birth control methods! So, the cycle continues: women read about terrible experiences and become too fearful to get an IUD, or if they do get one, their fear magnifies the pain.
Still, what many say they wish they had most is transparency. In interviews, people consistently noted that knowing more about the potential discomfort, possible complications, and range of outcomes would have helped them prepare better. The takeaway? If you’re considering an IUD, finding a provider who will talk you through the details transparently can make all the difference.
Does Your Doctor Even Care About You?
The answer is, for most patients, a resounding YES!
While there’s no denying that patriarchal and racist medical structures have shaped how women’s pain is dismissed (and those patterns still show up in research and lived experience), the vast majority of clinicians genuinely care about their patients and want them to have a comfortable, trauma-free IUD insertion. Many OB/GYNs deeply understand how painful an insertion can be and actively try to make it better. One OB/GYN, Dr. Shieva Ghofrany, put it this way: “We really care about women’s pain– we’re always trying to make this as easy as possible with the tools we have.”
So what does that look like?
They manage expectations, giving patients a realistic understanding of what will happen.
They strategize in advance, discussing pain-relief preferences before the procedure begins.
They explain each step, so the patient has agency instead of bracing for unknown sensations.
They slow down intentionally, pausing before inserting the tenaculum or sounding the uterus so patients can breathe and prepare.
They focus on consent and bodily autonomy, making sure patients feel in control and can say “stop,” “pause,” or “give me a second.”
Technique matters too: research shows that something as simple as applying the tenaculum slowly instead of with a quick clamp can significantly reduce pain. In other words, compassionate clinicians and a flawed system often exist at the same time.
This is why choosing a thoughtful provider: one who is patient-centered, slow, communicative, and collaborative, can dramatically shape your pain experience. So why don’t they offer more pain relief options? It often comes down to what is (and isn’t) covered by insurance, which is out of clinicians’ control.
Better Pain Relief, and Then a Sucker Punch
For over a decade, the Women’s Health and Fertility Branch at the Centers for Disease Control and Prevention (CDC) has been responsible for crafting national, evidence-based guidelines on contraceptive care. Their work has been especially vital for patients with complex conditions like cardiovascular disease, lupus, sickle cell disease, and obesity. These clinical recommendations helped providers navigate which birth control methods were safe for millions of women whose health profiles required extra consideration.
In August 2024, the same team released new guidance that explicitly urged providers to counsel patients on potential pain during IUD placement and offer tailored pain management options based on individual needs. The updated guidelines, part of the CDC’s Selected Practice Recommendations, also broadened the list of pain relief tools clinicians could consider during IUD insertion (more on this in A Quick Guide to IUD Pain Management Options).
Just months later, on April 1st, 2025 (and no, it wasn’t a prank), the entire CDC division responsible for this work was dismantled in a large-scale federal workforce reduction. The eight-person team behind what many clinicians considered the contraceptive care “bible” was abruptly fired. The CDC’s contraception app and other resources were taken offline, and with them went the institutional memory and expertise that had shaped national standards for over a decade. As one senior CDC scientist put it in an interview shortly after the cuts: “No one else does this work. Even [professional physicians’ associations] look to the CDC to do it. You lose this expertise, and it will be gone forever.” The 2024 update, once envisioned as just the latest in an ongoing series, may now be the final edition.
In 2022, the overturn of Roe v. Wade triggered a sharp spike in online searches for birth control options. With abortion access suddenly uncertain, more women turned to long-acting contraception (like IUDs) as a safeguard for reproductive autonomy. Now, the timing of these federal cuts couldn’t have been worse. With reproductive access already under threat in many states, the CDC team that had been making progress on issues like IUD pain has now ground to a halt.
No One’s Coming. Now We Step Up.
So what now? Where do we go in a post-guideline world, when the experts are gone but the need remains? With top-down leadership gone, the responsibility now falls on patients and providers to carry the torch together.
Clinicians can commit to staying informed through professional societies such as the American College of Obstetricians and Gynecologists (ACOG), which has underscored the need for improved pain management and adopted new guidelines. Meanwhile, patients can keep doing what they’ve already been doing: sharing their stories and speaking up for better care.
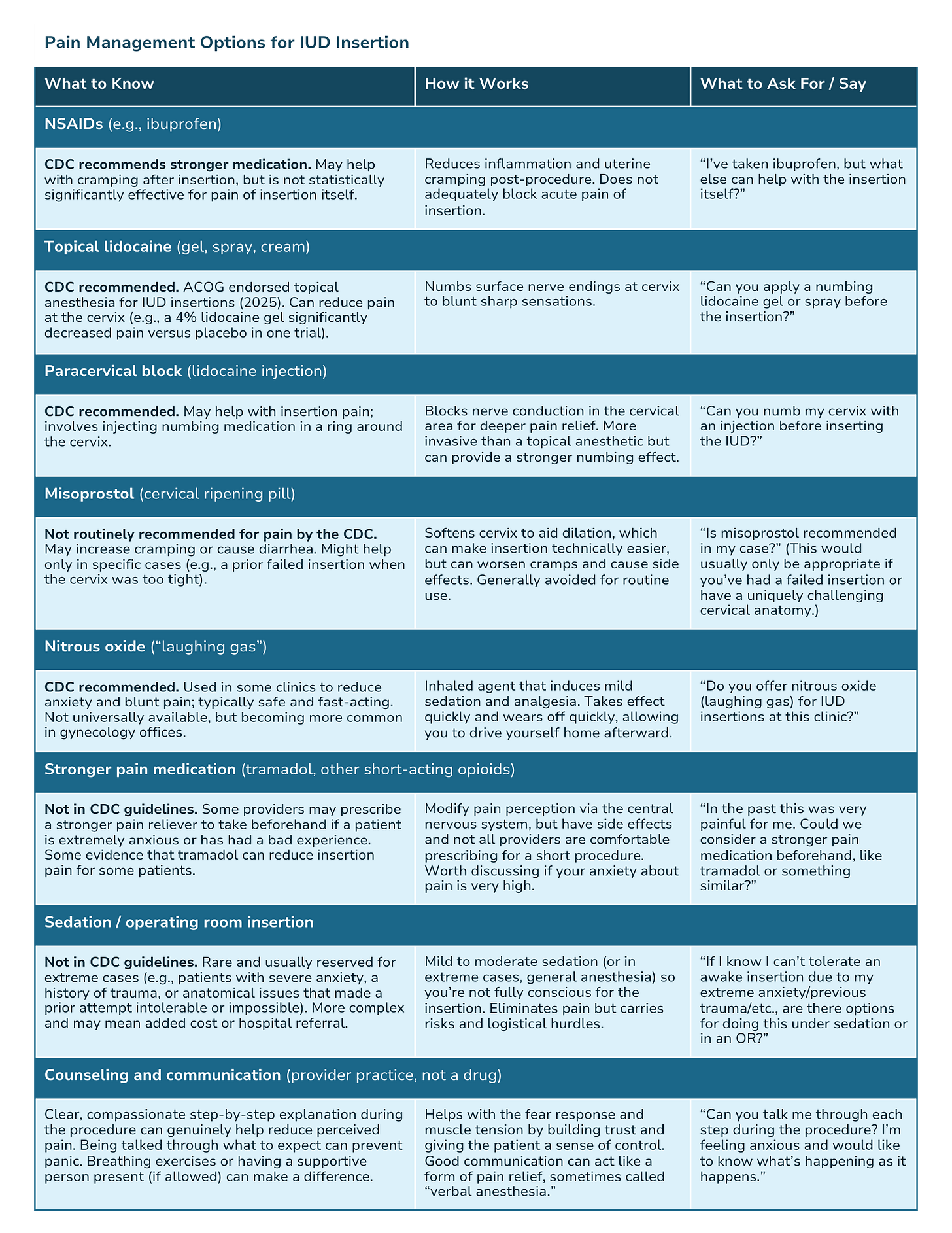
After reviewing the 2024 U.S. Selected Practice Recommendations for Contraceptive Use, one thing became clear: the evidence remains murky. Still, patients shouldn’t be left guessing. Here’s what you need to know, and what you can ask for to help you advocate for yourself at your IUD appointment.
A Quick Guide to IUD Pain Management Options
*Note: These medications may not always be available in every clinic. Some of these tools are expensive, and clinics often pay out of pocket or charge the patient directly to provide them. Still, it’s important to know your rights and ask your doctor about all available medications!
How to Prepare for Your IUD Appointment:
When you’re gearing up for an IUD insertion, going in prepared can make a huge difference in how the experience feels—physically and emotionally. Make sure to remember the following:
Providers MUST counsel you on pain:
The CDC explicitly states that clinicians must counsel you about potential pain and the full range of risk, benefits, and alternatives of pain-management options before the procedure. If your doctor hasn’t mentioned pain management, you can say: “The CDC guidelines say patients should be counseled about potential pain and options. Can we talk about that?”
Bring the pain-management table with you (a screenshot works perfectly!) and ask which options your clinic actually offers and whether they’re covered by insurance.
During the appointment, don’t hesitate to request a detailed, step-by-step explanation of what’s happening and ask your provider to guide you through the process in real time—this alone can make the pain feel far more manageable. For instance, you can say: “I’m pretty worried about the potential pain. What can we do to make the insertion more comfortable for me?” A good clinician will take that cue and discuss options. And if they dismiss your concerns or make you feel silly for asking, remember that you have every right to seek a second opinion or find a provider who will listen and prioritize your comfort.
If you’re anxious, say so. A supportive clinician will take that seriously, not dismiss it.
And finally, some OB/GYNs strongly recommend taking 800 mg of ibuprofen about an hour before your appointment. Remember, ibuprofen helps with uterine cramping because of its anti-inflammatory, prostaglandin-blocking effect—Tylenol won’t do this. Some providers will also prescribe a single dose of an anti-anxiety medication if you need it. These small steps, combined with a thoughtful provider, can meaningfully improve your overall experience.
Moving Forward
If there’s one takeaway from this piece, it’s that pain shouldn’t be the price of access. IUDs are an excellent option for birth control, but that doesn’t mean getting one should require grit or silence. The research is clear: tools like topical anesthetics, numbing injections, and supportive counseling can make a difference. And in 2024, the CDC formally recommended offering these as part of a shared, patient-centered plan.
But now, with the federal team behind those guidelines gone, there’s no one left to monitor whether the recommendations are being followed, or to keep updating them. That leaves the responsibility with us: with patients who speak up, and with providers who choose to listen. The information above is one small step toward helping that happen. Ask questions. Say what you need. Expect more.
When women are given all the information and options, their choices become clearer, and their care improves. The system slowly begins to change. We shouldn’t have to wait for someone else to fix this- the time to demand compassionate, informed reproductive care is now.
Stay Curious,
Unbiased Science


While I’ve never had an IUD I experienced exactly this with an endometrial biopsy for post menopausal bleeding. I was in no way prepared for the pain and cramping. I’ve never experienced anything like it. I was really traumatized and literally drove home tearful and in shock. I’m a now retired RN and I’ll never forget it.
I hope this brings great awareness to anyone considering an IUD.
While it can be a great option for some women, it was not right for me after I had my second child and knew I didn’t want any more kids.
For one, I had to pay out of pocket for it since my insurance wouldn’t cover it.
The placement of it was ok, no issues there. It was the after effects.
Let’s say I’m very sensitive to hormone changes.
I felt totally off all the time. I spoke with my doctor and he made nothing of it. I didn’t like it but gave it more time. However, I knew it wasn’t a way I wanted to feel everyday so I asked to have it removed a few months after placement.
My doctor was annoyed with me but he complied.
I went back to feeling “normal” after it was removed.
However, I was on a payment plan for $1000 and still had to pay it off.
No one ever mentioned that it could make me feel totally off, so if you’re sensitive to biochemicals, like hormones (or for me caffeine too), ask your doctor about that.
Thanks for reading!