Tick Tock: AI Joins the Race Against Sepsis
Every minute counts-- How AI is revolutionizing detection of America's 3rd leading hospital killer.
We came across a meme the other day that struck a chord. It showed AI being used to detect breast cancer, with a caption that read, "This is what we want AI used for, not to create another social media auto-replier for marketing." It got us thinking about the real potential of AI in healthcare, beyond the buzzwords and marketing hype we often see.
So, we are joining forces– Unbiased Science and TECHing It Apart– to pool our expertise in public health, data science, clinical medicine, risk assessment, and computer & electrical engineering– to explore the ways that AI is being integrated into healthcare.
While AI chatbots and content generators are grabbing headlines, some truly groundbreaking work is happening in medical technology. Today, we want to talk about how AI is making a difference in an area that doesn't always get the spotlight but affects millions: sepsis detection.
Sepsis: A Silent Crisis in Healthcare
Before we dive into the tech, let's talk about why this matters. Sepsis is one of those conditions that keeps healthcare professionals up at night. It’s a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs. Sepsis is responsible for over 270,000 deaths annually in the U.S. alone. To put that in perspective, that's more than the number of lives lost to breast cancer, prostate cancer, and AIDS combined. Globally, it causes about 11 million deaths every year.
Sepsis doesn't discriminate, but some groups are at higher risk: infants, the elderly, those with weakened immune systems, and recently pregnant women. It can stem from various infections, including (but not limited to) pneumonia, UTIs, abdominal infections, and skin infections. Symptoms range from fever and rapid heart rate to confusion and extreme pain. Treatment is complex, often requiring antibiotics, IV fluids, and intensive care support.
But here’s the issue… It's difficult to detect early due to nonspecific symptoms that overlap with other conditions. Diagnosis is often delayed due to reliance on slow diagnostic tools like blood cultures. And that’s where AI has come into the picture.
Evolution of Sepsis Identification and Management
Sepsis monitoring and management have evolved significantly over the past two decades, reflecting our growing understanding of this life-threatening condition. In the early 2000s, Dr. Emanuel Rivers revolutionized sepsis care with his Early Goal-Directed Therapy (EGDT) protocol, emphasizing aggressive fluid resuscitation and continuous monitoring. While groundbreaking, some aspects of EGDT have since been refined based on newer research.
Initially, clinicians relied on the Systemic Inflammatory Response Syndrome (SIRS) criteria to identify sepsis. SIRS looked at factors like body temperature, heart rate, respiratory rate, and white blood cell count. However, some SIRS criteria, like arterial blood gas measures, proved impractical and invasive for routine use.
Today, many clinicians use more streamlined tools like the Quick Sequential Organ Failure Assessment (qSOFA) to identify patients at risk for poor outcomes from sepsis. This tool, which looks at mental status, respiratory rate, and blood pressure, has largely replaced SIRS due to its simplicity and non-invasive nature.
Current sepsis protocols focus on early detection and rapid intervention, often employing "sepsis bundles" - sets of actions to be completed within a specific timeframe. These typically include lactate measurement, blood cultures, antibiotic administration, and fluid resuscitation within the crucial first hour after sepsis is suspected.
Despite these advancements, sepsis remains a significant challenge in healthcare, with high mortality rates and complex presentation. This is where emerging AI tools show promise, offering more accurate, timely, and personalized approaches to sepsis detection and management. In the following sections, we'll explore how AI is poised to transform sepsis care, addressing current limitations and opening new possibilities for improved patient outcomes.
Sepsis' New Nemeses? ImmunoScore and COMPOSER
Recent advances in artificial intelligence (AI) are revolutionizing the way healthcare providers diagnose and treat sepsis. Tools like ImmunoScore and COMPOSER are leading the charge, offering innovative solutions that promise earlier detection, more accurate diagnosis, and personalized treatment plans. It’s a science, technology, and healthcare trifecta.
What the TECH is AI?
Let's break down what we mean by AI. Artificial Intelligence refers to technologies that enable computers and machines to simulate human learning, comprehension, problem-solving, decision-making, creativity, and autonomy. At its core, AI learns from data using algorithms, creating models to make predictions or decisions.
(For a deep dive into the tech, including a basic introduction to AI, check out @techinginapart by @niniandthebrain.)
Key AI Concepts:
Machine Learning (ML): A subset of AI that focuses on building predictive models from data.
Deep Learning: A type of ML using artificial neural networks to model complex patterns.
Training: The process where AI learns from data to build its model.
Test Data: New, unseen data used to evaluate the AI model's performance.
AI for Sepsis: How the TECH does that work?
Ever wonder how AI tackles something as complex as sepsis detection? It's all about pattern recognition on steroids. AI excels at spotting patterns in massive datasets that might slip past even the most eagle-eyed human. For sepsis detection, AI analyzes vast amounts of patient data, including vital signs, lab results, and biomarkers. It can identify subtle patterns and relationships that typically precede sepsis, allowing for earlier detection and intervention.
For example, ML algorithms in sepsis detection might process:
Patient demographics
Vital signs trends
Laboratory results over time
Medical history
Current medications
By continuously learning from new data, these AI models can predict the likelihood of sepsis developing within hours - often before obvious clinical signs appear. It's like having a crystal ball, but one based on actual clinical data.
Image Source: Bhowmick, Nitesh. “ML Use Cases in Manufacturing.” Medium, 29 Jan. 2023, https://medium.com/@nitesh.gnit/ml-use-cases-in-manufacturing-b02774381556.
There are several FDA-cleared diagnostic tools for detecting infections, but most rely on single or multiple blood biomarkers. For example, Procalcitonin is a biomarker used to assess the risk of severe sepsis in critically ill patients. The IntelliSep Test measures leukocyte properties to identify sepsis with organ dysfunction within three days, while the Early Sepsis Indicator from Beckman analyzes monocyte width to gauge sepsis risk.
But here's where it gets really interesting.
Enter the Sepsis ImmunoScore by Prenosis – an FDA-cleared AI-based diagnostic tool that combines multiple inputs - demographics, vital signs, lab results, and sepsis biomarkers - to generate a comprehensive risk score. It’s designed to integrate with electronic medical records (EMR) to provide real-time diagnostic support when ordered by healthcare providers. Studies have shown that such AI-driven tools can reduce sepsis-related ICU admissions, shorten hospital stays, and lower overall treatment costs by preventing sepsis complications before they escalate.
By leveraging machine learning, ImmunoScore processes vast patient data to generate a personalized sepsis risk score in real-time. This score helps clinicians detect sepsis within 24 hours of patient evaluation, enabling timely interventions that prevent progression to critical stages like septic shock.
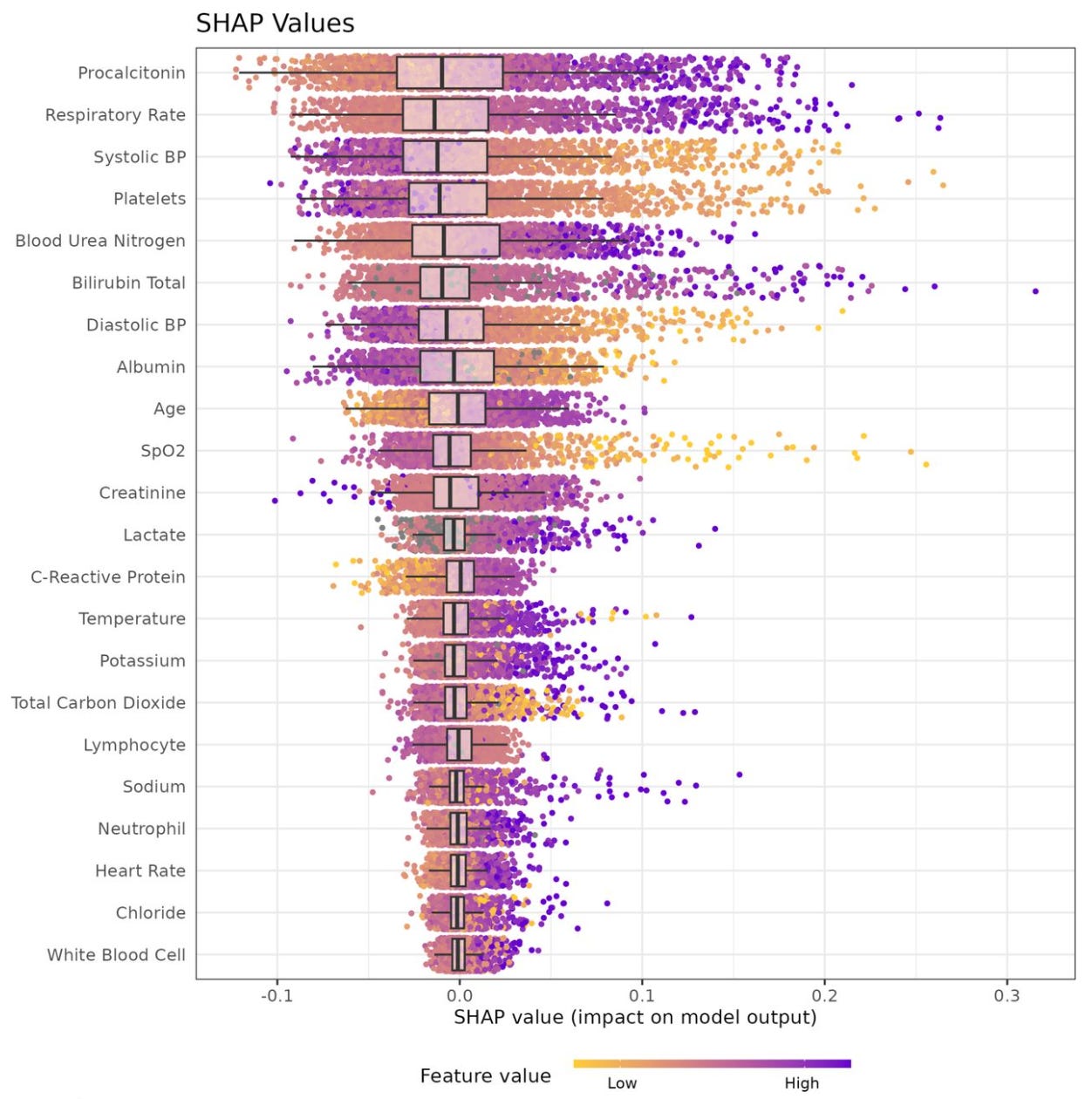
This image shows us what the ImmunoScore AI considers most important when predicting sepsis risk. Think of it as a ranking of medical clues, from most to least crucial:
Image source: Bhargava, Akhil, et al. Development and Validation of the First FDA Authorized Artificial Intelligence/Machine Learning Diagnostic Tool for the Prediction of Sepsis Risk. medRxiv, 16 Aug. 2024. medRxiv, https://doi.org/10.1101/2024.05.06.24306954.
What we're looking at:
Each dot represents a patient's data point
The further right a dot is, the more it influences the AI's decision
Purple dots show higher-than-normal values, yellow dots show lower-than-normal values
Grey dots are for missing data that the AI had to estimate
Key takeaways:
The most important factors are at the top of the list
Procalcitonin (a blood biomarker) and respiratory rate are major red flags when elevated
Low blood pressure and low platelet counts also raise significant concern
The AI considers a wide range of factors, demonstrating its comprehensive approach
This visual helps us understand how ImmunoScore processes patient data to assess sepsis risk, combining various medical indicators for a more accurate prediction.
Putting AI To The Test
The Sepsis ImmunoScore algorithm didn't just sound good on paper - it proved its worth in a rigorous real-world trial. From 2017 to 2022, researchers put ImmunoScore through its paces in a comprehensive multicenter study spanning five hospitals. They enlisted 3,457 participants, dividing them into groups to train the algorithm and then test its performance.
Here's how the study was structured:
Derivation Cohort: 2,366 patients were used to develop and train the algorithm.
Internal Validation: 393 new patients from the same hospitals were used to test the algorithm's performance.
External Validation: 698 patients from completely new hospitals served as the final test of the algorithm's capabilities.
For each patient, ImmunoScore analyzed 22 different data points, including demographics, vital signs, and lab results. The algorithm's task was to predict who would develop sepsis within the next 24 hours.
To measure ImmunoScore's performance, researchers used the Area Under the Curve (AUC) value. AUC measures how well the algorithm distinguishes between sepsis and non-sepsis cases. Values range from 0 to 1, with higher values indicating better performance:
0.5 indicates no discriminative ability
0.7-0.8 is considered acceptable
0.8-0.9 is excellent
Above 0.9 is outstanding
How’d ImmunoScore measure up? Drumroll, please…
Derivation cohort: 0.85 AUC
Internal validation: 0.80 AUC
External validation: 0.81 AUC
The ImmunoScore's AUC values (0.80-0.85) indicated excellent performance in predicting sepsis across different patient populations. This means the algorithm can accurately identify sepsis cases while minimizing false positives and negatives, potentially leading to more timely and appropriate interventions.
The model’s predictions were calibrated to align with actual probabilities of sepsis, and the results were divided into four risk categories based on severity (low, medium, high, or very high). They were also able to calculate the most important features influencing the model's predictions, providing insight into how the algorithm makes its decisions. (These were PCT, respiratory rate, and systolic blood pressure.)
ImmunoScore's De Novo FDA Approval
ImmunoScore received De Novo approval from the FDA, a regulatory pathway for novel medical devices with low to moderate risk that have no existing market equivalents. This approval indicates that ImmunoScore has met FDA standards for safety and effectiveness. It may also establish a regulatory precedent for future sepsis diagnostic tools.
COMPOSER: Another Approach to AI-Driven Sepsis Management
While ImmunoScore focuses on risk assessment, another AI tool, COMPOSER, takes a different approach to sepsis management. Developed at UC San Diego, COMPOSER has shown promising results in clinical studies:
Demonstrated a 17% reduction in sepsis-related mortality
Uses deep learning to analyze over 150 variables, including vital signs, laboratory results, and demographic data
Aims to predict sepsis onset before full manifestation
Provides continuous patient monitoring and early alerts for high-risk patients
A UC San Diego study on AI-based surveillance tools like COMPOSER reported:
Improved patient outcomes
Reduced mortality rates
Improved survival times and overall patient health
Real-time operation, allowing for faster clinical decision-making and potentially reducing time between diagnosis and treatment
Here’s a glimpse into the way COMPOSER integrates with the EMR– prompting clinicians about a patient’s sepsis risk score with clear action steps to confirm the diagnosis:
Image created by Unbiased Science
Adapted from: Ph.D, Dr Priyom Bose. “Deep Learning Model COMPOSER Enhances Early Sepsis Detection and Patient Survival.” News-Medical, 24 Jan. 2024.
Addressing the Barriers to Sepsis Diagnosis
AI-powered tools like ImmunoScore and COMPOSER are designed to address the key barriers in sepsis care:
Early Detection: Both tools leverage AI to identify the early signs of sepsis, enabling clinicians to act before the condition becomes life-threatening. COMPOSER and ImmunoScore go beyond traditional methods by using biomarkers and data analytics to provide real-time risk assessments.
Speed and Accuracy: Traditional diagnostics like blood cultures are slow and often too late for effective sepsis treatment. AI models analyze vast amounts of data at once, providing rapid, accurate assessments that significantly cut down the time to diagnosis.
Personalized Care: By using patient-specific biomarkers and clinical data, these tools offer personalized risk scores, which lead to more tailored treatment plans, reducing the likelihood of overtreatment with antibiotics and ensuring timely interventions.
Broader Clinical and Public Health Impacts
The potential for AI tools like ImmunoScore and COMPOSER to reduce sepsis-related mortality extends beyond individual patients. These technologies promise to alleviate the financial burden on healthcare systems by preventing costly ICU admissions, shortening hospital stays, and reducing the need for long-term rehabilitation. A 2021 study published in NPJ Digital Medicine highlighted that the early implementation of AI tools in sepsis care could result in substantial cost savings, with estimates showing a reduction in healthcare expenditures by billions annually.
Moreover, AI tools have the potential to transform emergency medicine as a whole. By providing rapid, accurate diagnoses, they could set the standard for managing other critical conditions like heart failure, stroke, and respiratory illnesses.
Challenges to Implementation
Despite the promise of AI in sepsis management, several challenges remain. Integration costs and training are significant hurdles for healthcare systems. Hospitals must invest in the infrastructure to support AI-based diagnostics and train clinicians to use these tools effectively. Additionally, while AI tools can streamline clinical workflows, they must complement, rather than replace, the clinical judgment of healthcare professionals.
Despite the promise of AI in sepsis management, several challenges remain:
Integration costs: Healthcare systems must invest in infrastructure to support AI-based diagnostics.
Training requirements: Clinicians need proper training to effectively use these new tools.
Workflow integration: AI tools must complement, not replace, clinical judgment.
Data privacy and security: Ensuring patient data protection in AI systems is crucial.
Potential for bias: AI algorithms must be carefully designed and monitored to avoid perpetuating or introducing biases in healthcare delivery.
Regulatory hurdles: Ongoing adaptation of regulations to keep pace with AI advancements in healthcare.
Addressing these challenges is crucial for the widespread adoption and success of AI in sepsis care.
The future of AI in healthcare is here.
AI's potential extends beyond sepsis detection. In breast cancer screening, AI algorithms have shown promise in improving the time to review the many scans being performed in our healthcare systems while also reducing false positives and negatives. AI is also being applied to predict heart disease, detect early signs of Alzheimer's, and create personalized treatment plans for diabetes.
These applications demonstrate AI's broader potential to transform healthcare by augmenting limited or overstretched radiology/doctor resourcing, improving diagnostic accuracy, enhancing treatment precision, and optimizing patient outcomes across multiple conditions. As AI technology continues to evolve, it promises to play an increasingly significant role in various aspects of medical care and public health.
The Promise and Challenges of AI in Sepsis Care
The introduction of AI-powered tools like ImmunoScore and COMPOSER represents a new frontier in sepsis care. These tools offer a faster, more accurate, and personalized approach to diagnosis and treatment, addressing many of the long-standing challenges in sepsis management. While barriers to adoption remain, the potential clinical and economic benefits are significant.
However, as highlighted in a recent interview conducted by renowned clinical scientist Dr. Eric Topol with Sayash Kapoor and Arvind Narayanan, co-authors of of "AI Snake Oil" (via Ground Truths newsletter and podcast), it's crucial to approach AI implementation in healthcare with both optimism and healthy skepticism. Topol and his guests discuss examples of AI failures in healthcare, including flawed COVID-19 prediction models and problematic sepsis detection algorithms. These cases underscore the importance of rigorous validation and ethical deployment of AI tools.
Yet, despite these cautionary tales, Topol also expresses optimism about the potential of generative AI and multimodal AI models in medicine. This aligns with our view: while AI holds great promise for improving sepsis care and other areas of medicine, it's crucial to approach its implementation critically.
As AI becomes more integrated into healthcare systems, it holds the potential to save countless lives and dramatically reduce the burden of sepsis on patients, caregivers, and society at large. However, we must remain vigilant about bioethical concerns, such as privacy issues, bias in algorithms, and potential misuse of data. These concerns highlight the importance of transparent, ethical AI development.
The future of AI in sepsis care – and healthcare in general – lies in striking a balance between leveraging its transformative potential and ensuring its responsible use. By doing so, we can harness AI's power to improve accuracy, reduce diagnostic errors, and speed up treatment decisions, ultimately saving lives and enhancing patient outcomes in critical conditions like sepsis.
-What The TECH? (A collaboration between Unbiased Science and TECHing It Apart)